In one of the starkest warnings to date the Independent Expert Group assessing Sri Lanka’s Covid situation is predicting an explosion of new Covid infections in the next three months and is calling for an immediate restriction of mobility and social mixing to save thousands of lives and ICU admissions.
The IEG, a collective of expert epidemiologists, public and community health specialists, immunologists and physicians, say that stricter levels of stringency similar to what was in place between May and June this year for four weeks will avert at least 18, 000 deaths by January 2022 because it will reduce deaths to less than 25 a day. If not, they predict a cumulative total of 30, 000 deaths by the same date. Tighter mobility controls will also reduce the number of daily infections by about 1000 and patients needing ICU care to less than 25 a day.
According to them, Sri Lanka’s daily Covid infections will rise to 6000 up to mid- September and the number of deaths will peak at about 220 up to early October if the current low level of mobility restrictions continue. They chillingly point out that the number of ICU admissions will also peak around 275 by early October.
A four- week respite will help accelerate the vaccination drive, give the population time to develop their protection after the second dose of the vaccine and for the health system to recover from the crushing caseload they are having to deal with.
The IEG, which met on the 10th of August for this latest review, based their alert on projections carried out by the University of Monash in Australia in collaboration with the WHO Regional Office for South-East Asia and its country office in Sri Lanka. The data on cases and deaths which they used was that of the Epidemiology Unit of the Ministry of Health.
Painting an even bleaker picture they point out these projections are based on an assumption that 50% of Sri Lanka’s population will be fully vaccinated by end August 2021. However, since the vaccine coverage is not at the level assumed by the model, the projections are an underestimate which means the number of infections, ICU admissions and deaths will be much higher. As of Wednesday, only 16. 8 percent of the Sri Lanka’s population had received both doses of the vaccine.
The IEG’s wake- up call comes because of what they say is a ‘current surge in Covid 19 which has nearly overwhelmed the capacity of the health systems to provide the required adequate care for people’. Sri Lanka is a ticking bomb and could soon face a health crisis of unprecedented proportions.
Their assessment of the current situation is that the country is showing a rapid increase in the daily reported number of cases and deaths (111 deaths reported on 09 August 2021 representing a doubling of deaths in a short space of time). They also noted that bed occupancy rates at all levels of care facilities (over 85%) and ICU’s (over 90%) have increased progressively and is now in full capacity. Because the number of patients who are dependent on oxygen have significantly increased from 528 last week to 646 patients on 9th August, they caution about an inevitability of a serious shortage of oxygen supply and interruption of care if the trend continues.
They also observe that many areas of the country show a high PCR test positivity rate of over 20%. As of 31 July 2021, more than 60% of sequenced samples are Delta variant, which is highly transmissible with a shorter incubation period. The Delta variant is now the dominant variant in the Western Province and will soon spread to other areas. The crisis will magnify once it spreads countrywide because most of the other provinces are not as well vaccinated as the Western province.
According to their assessment, for the vaccine that is used most widely, community vaccination will take 2-3 weeks after the second dose to provide adequate protection from severe disease and death. The newly vaccinated, single-dose vaccinated or unvaccinated groups are at very high risk of severe illness and it is very likely that there will be a further increase of cases and deaths, particularly in densely populated areas.
The IEG found that a significant number of health workers are getting infected with a consequent pressure for curtailment and closure of services which is an indication that the staff are exhausted and struggling.
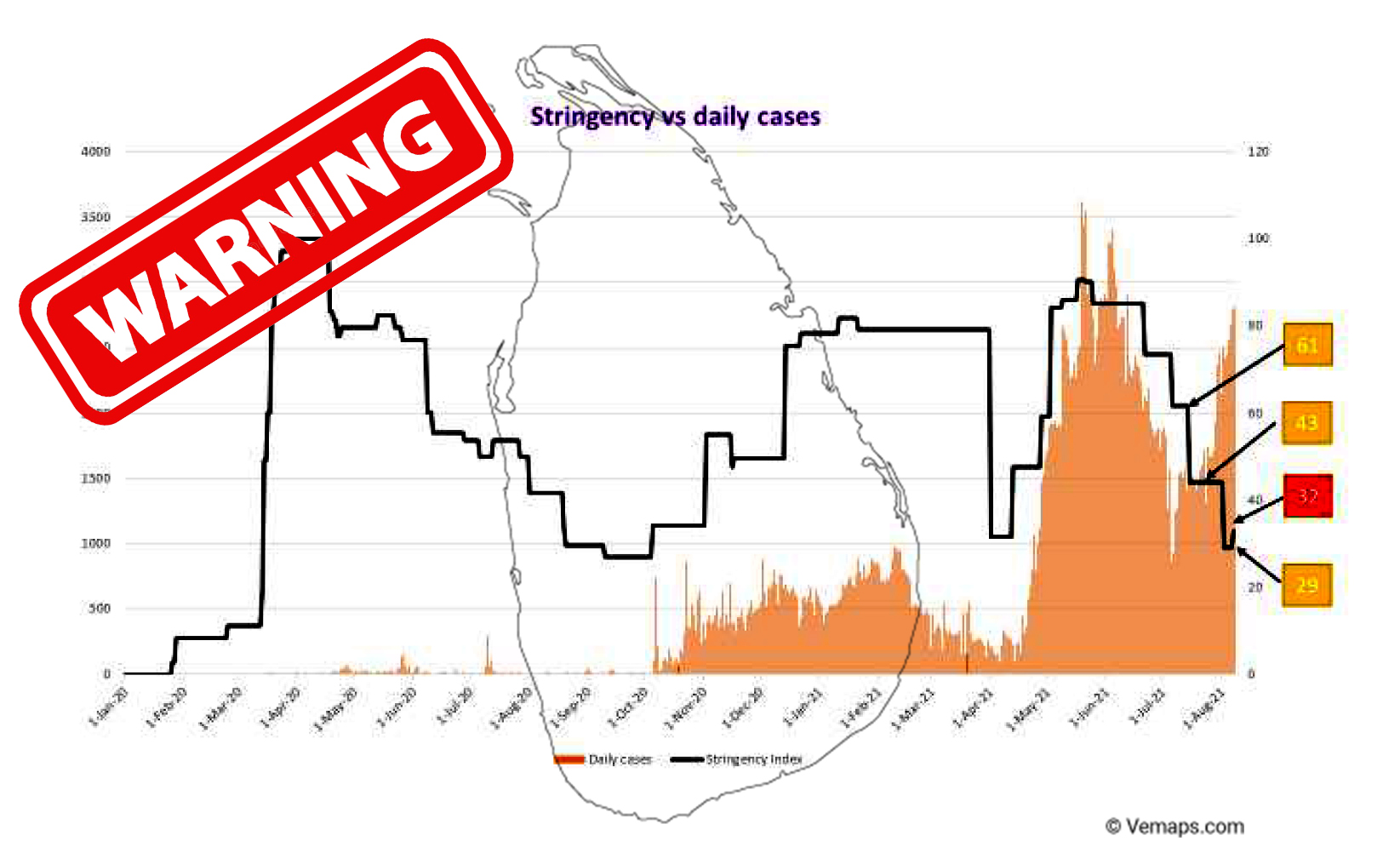
They note that in the midst of this situation, there is a sustained and high level of mobility and social mixing among the population despite nationwide restrictions (Oxford ‘Stringency Index’ was 85% (i.e. very effective restrictions in movement) in May, 49% in July and 29% by this week (i.e. dangerously low levels of movement restrictions).
The IEG came up with several recommendations to prevent the spread of the virus. Among them is the strict enforcement of movement restrictions, including inter-district travel except for essential services, which will be key. The effective implementation of these measures may require the enforcement of a curfew for a short period, in large geographic areas or nationally and restricting or cancelling all public events for three weeks. The also recommend the provision of care and protection to health workers and to augment staffing in hospitals to minimize disruption of essential health services.
Developing and implementing an effective communication plan to engage the public and to update them on the control measures and encouraging accurate reporting of both cases and deaths to get a better picture of the ground situation using proxy indicators such as observed Test Positivity Rate (TPR), trends measured using weekly moving averages and time series analysis, mobility data, etc is another recommendation they make. Prioritizing the vaccination of all those over 60 years old and those with co-morbidities, preferably with Pfizer, Moderna or Astra Zeneca is another recommendation which they make because even a single dose of these vaccines provides some degree of protection until the second dose is given.
The IEG underscores the cruciality of immediate action because it takes a few weeks before measures show a positive impact on the number of infections and hospital admissions. They point out that any delay in implementation will lead to an increase in deaths and will require even more stringent measures with a longer duration to regain control.
The Independent Expert Group consists of Dr Nihal Abeysinghe, President of the College of Community Physicians, Dr Vinya Ariyaratn,e a community health specialist, Professor Asita De Silva who is the President of the Association of Clinical Pharmacology and Therapeutics, Dr Rajiva De Silva, head of the Department of Immunology at the MRI, Dr LakKumar Fernando, President of the Association of Medical Specialists, Dr Padma Gunaratne, President of the Sri Lanka Medical Association, Professor Saroj Jayasinghe, Consultant Physician at the University of Colombo, Professor Indika Karunathilake former President of the SLMA, Professor Neelika Malavige, head of Department of Immunology and Molecular Medicine at the University of Sri Jayewardenepura, Professor Malik Peiris, Chair School of Public Health at the University of Hong Kong, Lalini Rajapaksa, Emeritus Professor of Community Medicine at the University of Colombo, Athula Sumathipala, Professor of Psychiatry at the Keele University and Professor of Global Mental Health at Kings College, Manuj Weerasinghe, Professor of Community Medicine at the University of Colombo, and Dr Ananda Wijewickrema past president of the College of Physicians. Among the WHO team which was present were Dr Alaka Singh who is the WHO representative in Sri Lanka, Dr Paba Palihawadana, Dr Olivia Nieveras, Dr Sapumal Dhanapala, Dr Padmal De Silva and Dr Palitha Abeykoon who is the WHO Director General’s Special Envoy for Covid 19 Preparedness and Response for SEAR. (SW)
Full Report – Independent Expert Group Recommendations 11th August 2021