Health sector professionals are accusing government bureaucrats for the shortage of medicines and medical equipment which triggered the current crisis crippling the health service.
‘The Ministry of Health has a clearly laid out procedure to assess stocks of medicine and essential health supplies that are needed every year’, said Ravi Kumudesh who is the President of the Academy of Health Professionals. ‘The assessment for the following year is usually carried out by December the latest of the previous year. People are now having to face the resulting crisis of policy decisions not having been made at the right time plus arrogant policy decisions made by a few who are in control’.
Although the forex crunch has played its part in the pinch these professionals point out that it has been in the making for a few years and that warnings went unheeded. Dr Sanjay Perera, an expert on pharmaceutical and healthcare management points out how in 2021 the tender for supplies was called 23 times, affecting the availability of this year’s supply. As many as 150 medicines could run dry in the coming weeks.
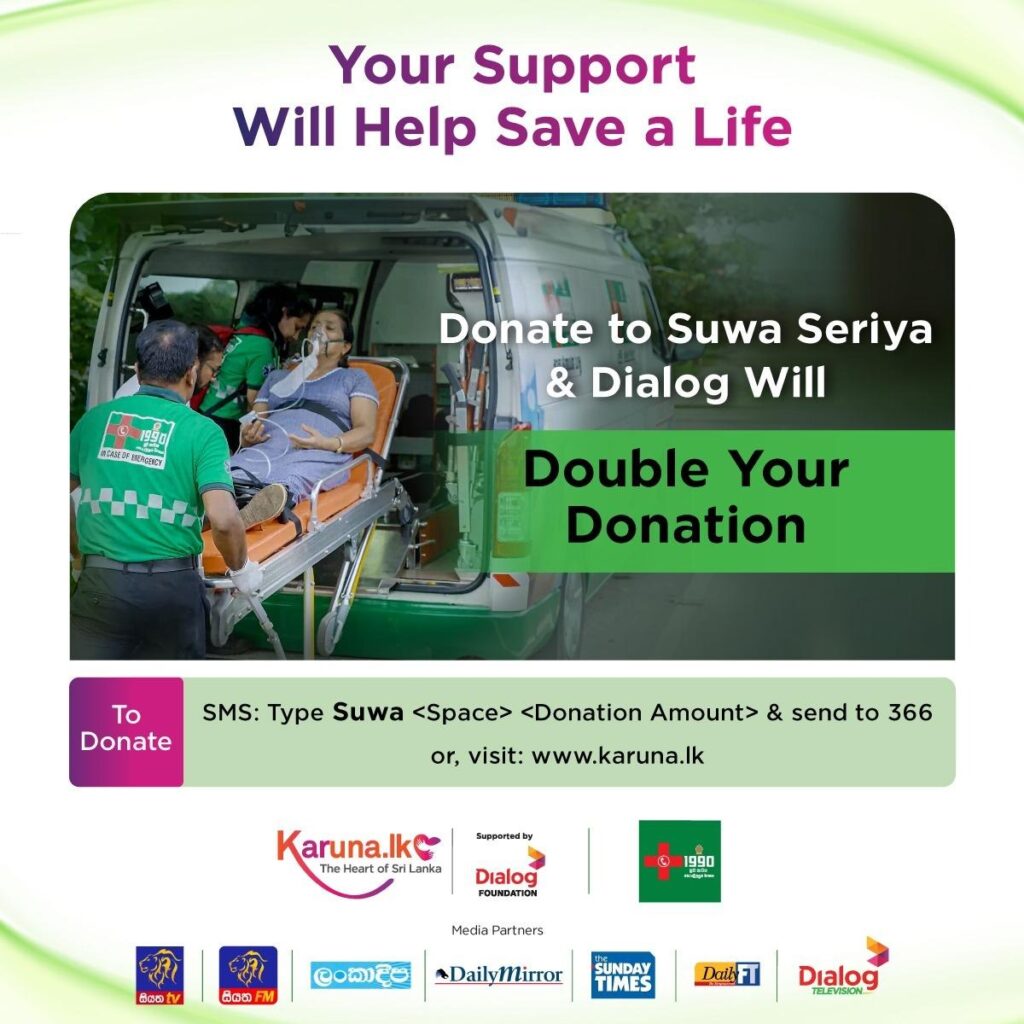
The health service is currently being drip fed by international donors and donations from the Sri Lankan expatriate community to buy critical and life– saving medicines and medical equipment. It runs the risk of a complete collapse if this in-kind assistance dries up. Sri Lanka has about an 800– strong hospital network which includes national, base, rural and maternity care centers.
Among the critical and life –saving medicines that are not available are those which are used to treat cancer, heart and brain ailments and liver failure. The availability of the anti –rabies serum which is given only in government hospitals, the tetanus and anti– venom treatment for snake biteare unclear and analgesics, antibiotics and anesthetics are reportedly hard to find. Health professionals are alert about a looming shortage of rare blood groups because of insufficient blood bags. In the grip of these shortages, hospitals have put off routine operations.
Successive statements by the Government Information Department quoting the Health Ministry about the situation have been at oddsand prevented a clear picture from emerging. On the 12th of April a statement from the Information Department denied there is a shortage of medicines and medical equipment but another on the following day admitted there is a shortage and appealed for donations.
‘As of now, we must accept the fact of a shortage of essential, critical and life -saving drugs’, said Dr Anver Hamdani, the Director of Medical Technical Services at the Ministry of Health who was recently appointed it’s focal to coordinate donor contributions.
Earlier this month the Director General of Health Services issued a circular appealing to donors to channel their contributions to the ministry and not to the donor’s chosen hospitalwhich used to be the practice. While this will be a new way for donations to be made, it will also help to centralise and streamline donations.
An initial World Bank grant of USD 10 million which has already been given to the Ministry of Health will be followed by another grant of USD 13 million. According to Dr Hamdani, USD 150, 000 has been pledged by the donor community in Singapore and a donation of medicines for USD 600, 000 from the government of Indonesia arrived last week. Among the Sri Lankan communities that have come forward to help are those in Thailand, Bangladesh and China. These donations will be used to bridge the gap as part of a wider plan to salvage the dying health service.
Some hospitals like the Lady Ridgeway Teaching Hospital, which is the country’s premier hospital for treating children, appealed to well wishers for medical equipment for general theater and surgical ICU and has already received them from Sri Lankans living in the UAE. The teaching hospitals in Kurunegela, Ragama and Rathnapura have also received donations from the expatriate community there.
Dr Perera foresees this crisis also paving the way for fraud. ‘Stocks of medicine and equipment will be allowed to deplete so that their purchase can be done out of the government’s tender process and through unregistered suppliers. It will also lead to purchases that are not approved by the National Medicines Regulatory Authority where efficacy is not guaranteed’.
Emergency purchases of medicines will also end up costing more. According to the observations of doctors in the Medical and Civil Rights Professional Association, emergency purchases can cost 1300 percent more and because of the volume of medicine that will be needed will stretch the country’s foreign currency reserves. ‘This can be as much as what the country has to pay towards its monthly external debt repayments’, it said in a statement.
Kumudesh says the government must declare a health crisis and appoint an expert committee to navigate the country out of this crisis. ‘The health minister and the secretary to the ministry do not have the capacity to do the work that has to be done in the ministry. What is needed is innovative thinking and a strategic and financial plan. The post of secretary to the ministry is a responsible one. The current secretary is from the military and is a political appointee. We need a medical doctor as a health minister’.
He also says the government must ask for humanitarian assistance from the UN.
Dr Hamdani meanwhile says he has submitted a three point plan to ministry officials to address the current crisis. The first step of the plan is to bridge the gap with the support from the Sri Lankan expatriate and diplomatic communities and the World Bank.
The second step according to Dr Hamdani will be to liquidate the Indian credit line to purchase the drugs which are needed. ‘We have started the administrative procedure for this already’.
The third step will be to work out a health plan which is financially sustainable and will engage the people.
Dr Hamdani is optimistic about the crisis easing off in the coming weeks if work is carried out according to the plan he has put forward. He is confident he will get the support of senior health ministry officials for it.
Kumudesh points out that the Indian credit line will be used to purchase generic drugs which constitute only 20 percent of the country’s drug use. The balance 80 percent are the preferred branded drugs which are of a higher efficacy. ‘These drugs, purchased from countries like Germany, are more expensive and the availability of these with the economic situation the way it is, is questionable’.
‘Now it’s a case of the care service having to adapt to the treatment that can be given instead of giving the best treatment that should be given. Patients who can be saved from death can die, patients without complications will develop complications and patients who can be cured of a disease can fall prey to disease’, says Kumudesh.