“Nun’s office Tivoli safe!” When I was a child, we used to play a game where several of us whispered a message to one another in sequence. The fun of the game is when errors pop up along the way – and the final listener announces with glee something quite different from the original message.
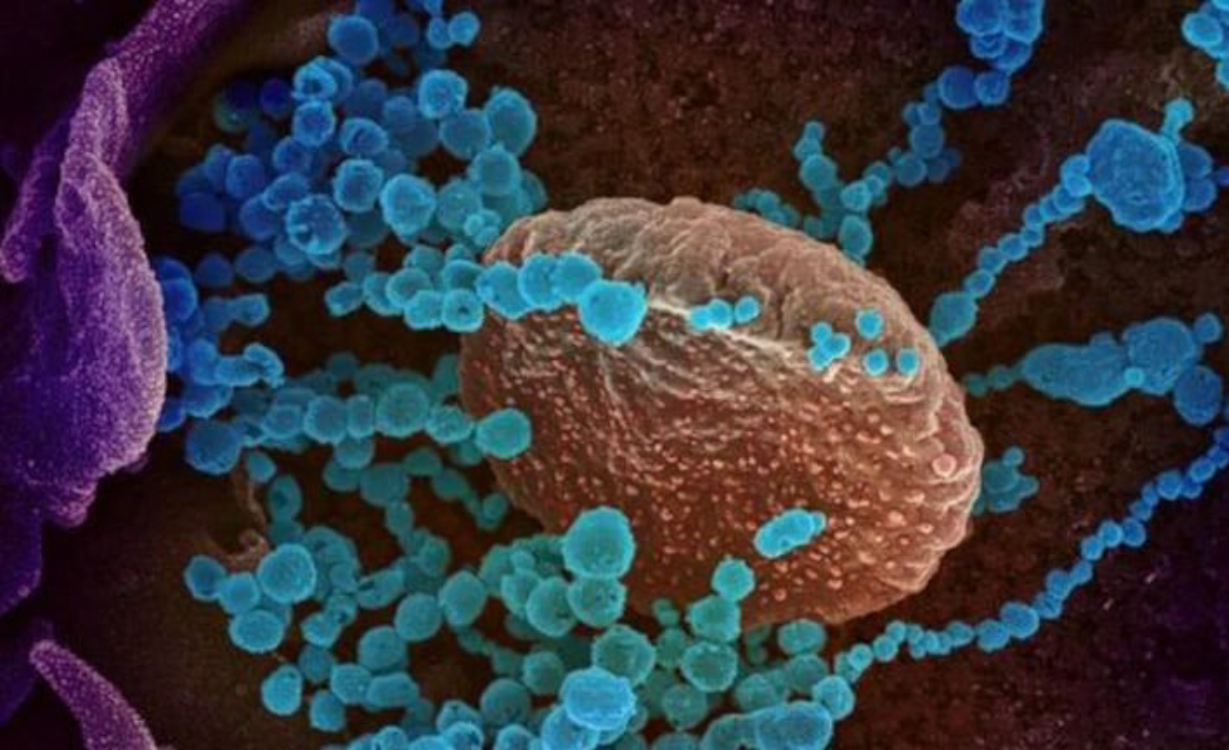
As Covid-19 spreads through a population, it undergoes similar changes, or “mutations”. Every time a new virus is built, errors are made when its genome is copied, just like with the whispered message. This has led to Covid-19 variants popping up all over the globe: in the UK, Brazil, the US and now India. Detecting these variants and monitoring their spread is crucial to protect people from being put at risk, and helps inform public health decisions. Which is why we so enthusiastically welcome the news of the Global Pandemic Radar, a pathogen surveillance network that will track developments in the Covid-19 virus. It will also ensure a global infrastructure is in place to better help humanity understand and protect itself from future pathogens.
Molecular epidemiology is a cutting-edge area of research in which scientists examine the genomes of viruses to understand their patterns of spread. The overwhelming majority of mutations have no effect on how the virus behaves, but the trail of mutations that accumulate in viruses as they are transmitted are signatures that allow us to retrace the virus’s steps. One signature might say “I am part of a local outbreak” while another could indicate an import from a specific region or country. We can’t tell who infected whom from virus genomes, but we can get a peek into where a virus has been and how it is moving through the population. We can answer questions such as: “When did this variant emerge?”, “How fast is it spreading?” and “Are current restrictions sufficient?”
Some mutations endow the new virus with a specific advantage, making it more transmissible, or allow it to hide from the immune system. We name mutations such as this “variants of concern”. The results from molecular epidemiology can be used to deploy public health resources effectively, for example by blocking variants of concern before they cause large outbreaks – and tweaking vaccines to better protect us.
A healthcare worker takes a nasal swab sample to test for Covid-19 in Santiago, Chile. Photograph: Esteban Félix/A
The scale of genetic sequencing during the Covid-19 pandemic, and the efforts to share those data, are unprecedented. Sars-CoV-2, the virus that causes Covid-19, has rapidly become the most sequenced pathogen in all of history – a position previously held by HIV. More than 1.5 million Covid-19 patients globally have had their virus sequenced and the data shared publicly through Gisaid, a database launched in 2008 following the first global outbreak of bird flu to log variants of influenza. In the same way as the second world war spurred on the development of technologies such as radar, the pandemic has led to astounding advances in how scientists generate, share and analyse virus data.
In the UK, sequencing efforts are coordinated at the national level through the Covid-19 Genomics UK (Cog-UK) consortium. Cog-UK was conceptualised in March 2020, when fewer than 100 Covid-19 cases had been diagnosed in the UK. Because molecular epidemiology played such an important part in mapping the spread of Ebola in west Africa in 2013-2016, and it was clear to scientists that genomic surveillance viruses should be a keystone of the UK Covid-19 response. At least 10% of Covid-19 positive samples are collected by Cog-UK from testing sites, hospitals and care facilities. Sequencing is then conducted in hubs across the UK. This systematic approach can reveal the genetic makeup of viruses circulating around the country. When UK cases surged in November 2020, despite lockdown restrictions, we rapidly pinned down the highly transmissible Kent variant (B.1.1.7) as the cause.
Some countries, such as the US and India, also initiated national Covid-19 genomic surveillance programmes. The Indian variant (B.1.617) was first identified through the Indian genomic surveillance system, Insacog, in October 2020. B.1.617 has mutations that increase transmissibility, and that may help it evade the immune system. Because of this, the WHO classified it as a variant of concern on 10 May. But it remains difficult to calculate its relative transmissibility and contribution to the current onslaught of infections in India, because sequencing has been patchy.
In most countries, sequencing efforts are even less systematic, and led mainly by labs that happened to be set up for pathogen sequencing prior to the pandemic. Academic institutions and hospitals are independently sequencing samples from their local areas, usually obtained from hospitals. In many lower- and middle-income countries, the only sequencing facility is in the capital and this means that only individuals living in the capital, or travelling there for treatment, ever get their virus sequenced. The UK has sequenced 50 out of every 1,000 diagnosed cases, compared with fewer than 1 in 1,000 in India. Eighty countries have submitted fewer than 100 sequences, which is insufficient for tracking variants.
While recent advances in the field are nothing short of a triumph, sampling and sequencing efforts remain a global patchwork. Uneven sampling can bias the results of molecular epidemiology, making it impossible to identify the geographic origin of a new variant and difficult to assess its transmissibility. Coordination of Covid-19 sequencing internationally by WHO was already underway, before the announcement regarding the Global Pandemic Radar. But laboratories must be equipped in key locations and staff trained so that procedures are consistent. However, global genomic surveillance for Covid-19 presents unique and daunting challenges. Not least that the sequencing will have to be both global and in real-time – unlike that which goes on for HIV and influenza. And sampling strategies may have to be adapted to address issues about which we are not yet even aware.
And what of “Nun’s office Tivoli safe”? “None of us is safe until everyone is safe”– one of the tag lines for the Covid-19 pandemic. The UK’s incredible sequencing efforts will be rendered pointless if global genomic surveillance remains so uneven. In contrast to the second world war, we are now united against a common enemy, and true cooperation is our greatest weapon against the virus.(Courtesy the Guardian of the UK)
Dr Manon Ragonnet-Cronin is an MRC Fellow at Imperial College London and a member of the Imperial College Covid-19 Response Team